The Link Between Oral Health and Systemic Diseases: What Science Says
For years, oral health was regarded as a separate entity from overall health. However, a growing body of scientific research is underlining the significant connection between the health of our mouth and the overall wellness of our bodies. The mouth is often considered a window to the rest of the body, providing signals of systemic diseases or conditions before they become more overt.
Today, we explore the intriguing links between oral health and systemic diseases, with a particular focus on heart disease and diabetes, relying on insights from two respected sources: the National Center for Biotechnology Information (NCBI) and Harvard Health.
The Mouth-Body Connection
The mouth is filled with numerous bacteria. With good oral hygiene practices, these bacteria are typically harmless. However, without adequate dental care, bacteria levels can grow to cause infections such as tooth decay and gum disease. But how does this affect the rest of our body?
Infections and inflammation in the mouth can provide a gateway for bacteria to enter the bloodstream. Once they're in circulation, these microbes have the potential to initiate and exacerbate systemic conditions.
Oral Health and Heart Disease
According to an article from Harvard Health, there's an evident connection between gum disease (periodontitis) and heart disease. But how does this link manifest?
- Inflammation: Gum disease increases inflammation in the body. Inflammation plays a crucial role in atherosclerosis, the buildup of fatty deposits in the arterial walls. This can lead to heart attacks and strokes.
- Bacterial Spread: The bacteria that cause gum disease can travel to the arteries and contribute to the formation of arterial plaques. These plaques can obstruct blood flow and potentially cause heart attacks.
- Endothelial Dysfunction: Research from the NCBI points to the potential of oral pathogens causing dysfunction in the endothelial cells, which line the walls of blood vessels. This dysfunction can lead to arterial diseases.
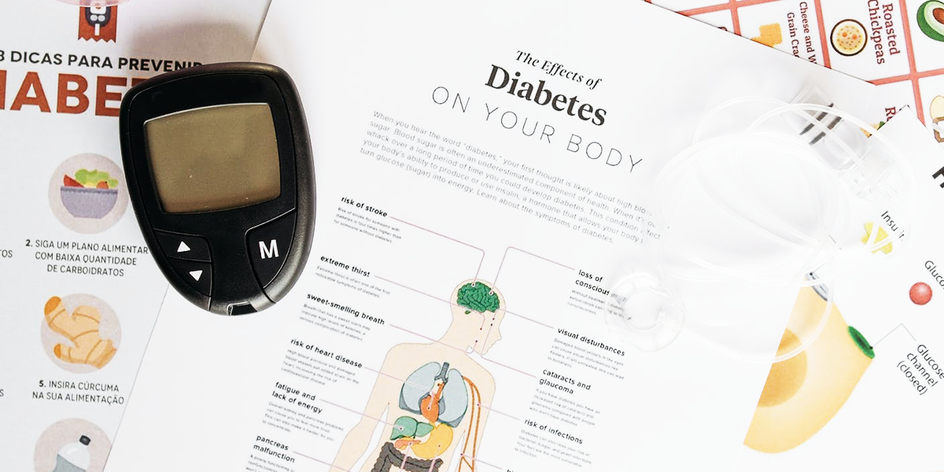
Oral Health and Diabetes
Diabetes and oral health share a two-way street of influence. While diabetes can increase the risk of developing gum disease due to decreased resistance to infection, gum disease can also complicate diabetes by affecting blood sugar control.
According to the NCBI study:
- Elevated Blood Sugar: The presence of gum disease can elevate blood sugar levels, making it harder for people with diabetes to manage their condition.
- Increased Risk of Complications: Those with diabetes and concurrent oral health problems face a higher risk of diabetic complications.
Beyond the Heart and Glucose Levels
While heart disease and diabetes are two primary systemic diseases associated with oral health, the list doesn't end there. Other conditions that may have links with oral health include:
- Respiratory Diseases: Oral bacteria can be aspirated into the lungs, potentially causing or exacerbating lung conditions like pneumonia.
- Pregnancy Complications: Gum disease might increase the risk of premature birth and low birth weight.
- Rheumatoid Arthritis: The NCBI notes that those with gum disease often have a more severe form of rheumatoid arthritis.
Prioritize Oral Health for Overall Wellness
The science is clear: oral health is intrinsically tied to our overall health. By maintaining a healthy mouth, we are not only safeguarding our teeth and gums but also offering protection against systemic diseases that can significantly impact our quality of life.
As such, regular dental check-ups, brushing, flossing, and a balanced diet are more than just recommendations—they are necessities for ensuring comprehensive health.
Stay informed, prioritize your oral health, and understand that the state of your mouth offers more insights into your health than you might have initially thought.